Do You Have Runner’s Knee?
“Runner’s knee” refers to one of two common1 repetitive strain injuries of the knee, either iliotibial band syndrome (knee pain on the outside) or patellofemoral syndrome (knee pain on the front of the cap).
Both conditions are common in runners, CrossFitters, triathletes, hikers, soccer players, and serious walkers. Unfortunately, they can be tough to tell apart. This quick guide will help you figure out which type of runner’s knee you have and give you some actionable ways to start fixing the issue.
There are many other causes of knee pain, but most knee pain in athletes who run often is one of these two.
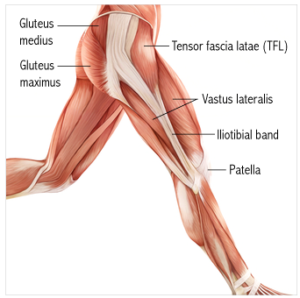
- Iliotibial Band Syndrome (ITBS) — Usually causes pain on the side of the knee. Also often called iliotibial band friction syndrome. The IT band is a vast tendon-like structure on the side of the thigh and knee (bad news, it still can’t be stretched or foam rolled). When the muscles upstream of it get tight, it will cause the insertion point around the knee to rub over the bone, which frays the tissue and causes pain.
- Patellofemoral Pain Syndrome (PFPS) — Usually causes pain on the front of the knee, around and under the kneecap. PFPS is more common than ITBS and more common in non-runners than ITBS. Although it primarily affects runners, hikers, and cyclists, it also affects anyone who sits for a living — the kneecap can be fatigued by a constantly flexed knee. It’s also quite common in teens.

How To Tell Which Version Of Runner’s Knee You Have
The easiest way to tell the difference between the two conditions is simply by the location of the symptoms. Patellofemoral Pain Syndrome affects the kneecap and surrounding area, whereas IT Band Syndrome affects the knee’s side (the side facing outwards).
What Causes Runners Knee?
Science doesn’t have an answer for what causes either condition. Most of the risk factors are unclear. Nearly every popular idea — such as hip weakness or “imbalances” — is someone’s unproven pet theory, often to “explain” the treatment they are selling.
We only know for sure that the risk of both injuries goes up with training volume, and both are more likely to affect inexperienced runners.
Almost everything else is speculation or wishful thinking. But there are a couple of safer bets based on the research.
#1. Slower Runners Get More IT Band Syndrome: Interestingly, if you run slow instead of fast, we know that it increases your likelihood of getting IT Band Syndrome. The data shows if you run at a cadence slower than 180bpm, it increases the chance you will get IT Band Syndrome.
#2 Heel Striking Hurts: Studies conducted by the military on running injuries also found that those who heel strike (heel hits the ground first) have a higher chance of getting IT Band Syndrome.
#3 Hills Make For Hot Knees: As far as Patellofemoral Pain Syndrome goes, climbing hills will cause it to flare up while going down hills can cause IT Band Syndrome to flare.
How To Know If Your Problem Is Not Runner’s Knee
Below is a list of symptoms that indicate an issue you should see a doctor for.
- Locking, clunking, or instability is usually an indication of another problem, typically trouble with the meniscal cartilage.
- Swelling is never a symptom of ITBS alone and rarely of PFPS. If you are swollen, something else is going on that is usually more severe.
- Sudden onset of symptoms — what I call an “oh shit moment” — usually indicates a traumatic mechanism. Neither ITBS nor PFPS starts that way. They can ramp up fast — as quickly as a few minutes — but not suddenly with a surge of pain.
- Throbbing pain in the back of the knee (or anywhere else) is almost certainly another issue.
- Tingling or numbness are never signs of ITBS or PFPS alone. If your knee is tingling or numb, and you haven’t been taking LSD, please see a doctor.
- Pain in the tendon under the kneecap — connecting the kneecap to the top of the shin — is probably just tendinitis. Pain in tendons usually is. (If you have patellar tendinitis, ITBS and PFPS should come to ASR to get treated. It’s in our wheelhouse of soft tissue issues).
What Can You Do About Runners Knee?
- Temporarily reduce your volume. Reducing volume can be challenging if you are in the middle of a training cycle for a race. That being said we know that taking time off and then slowly ramping back up works.
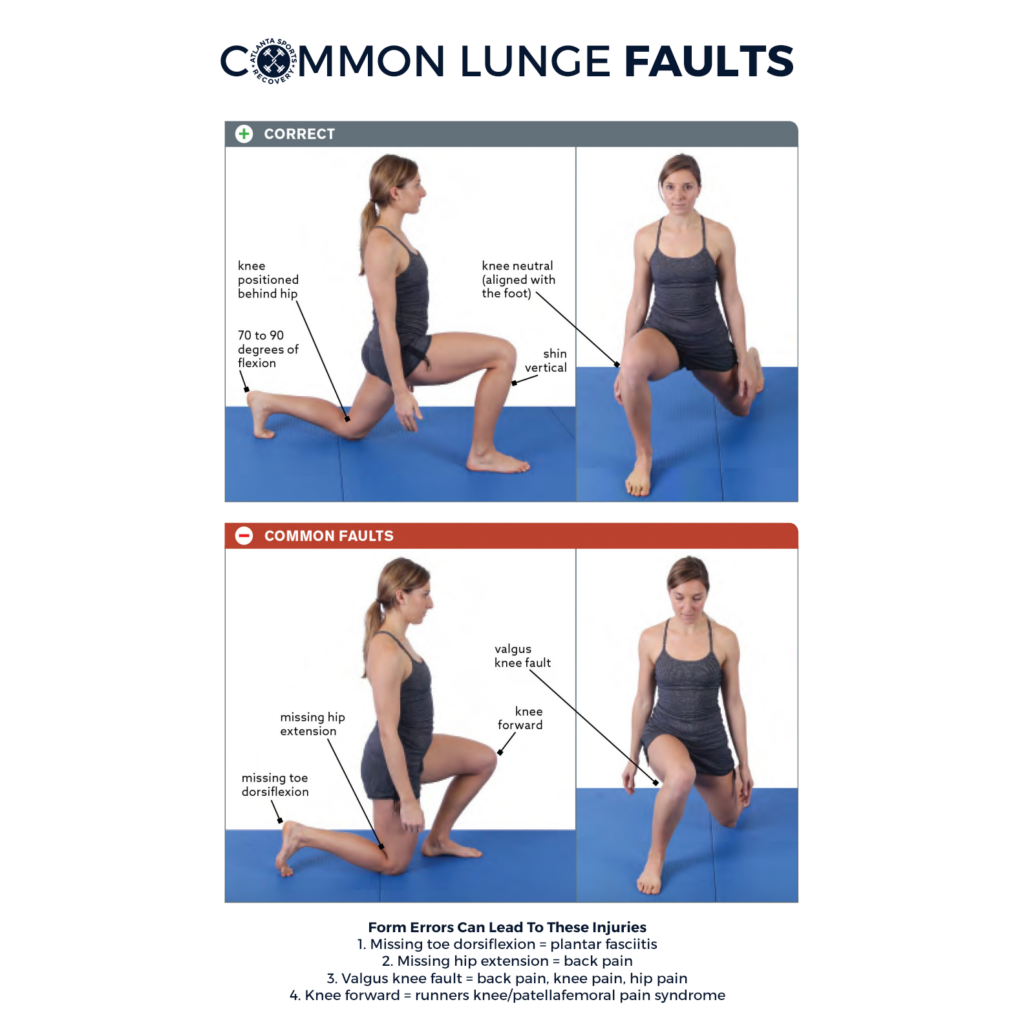
- Check your form. If you have improper form, you will be hurt. Heel striking and over striding will create knee pain. If you need help with your gait you should consider doing some running coaching with Johnny or Amanda.
- Voodoo Band your knee. The voodoo band is the best tool in your arsenal for desensitizing the pain generators and decongesting the lymphatic system so you can get the garbage out and bring new groceries into your tissues. Here is a video on how to use a voodoo band.
- Mobilize the up and downstream tissues with a Lacrosse Ball. When you have runner’s knee, all adjacent tissues are generally tight. Mobilizing your quads, hamstrings, TFL, calf muscles, and anterior tibialis will create slack in the system, which will loosen the mechanical tension on your knee, often reducing the pain. The increased blood flow will also help you heal faster. (click the links to see how to mobilize each muscle)
- Stretch. After you do a number on yourself with the LAX ball, stretch out your quads, hamstrings, and calves. It will help restore the natural length to your tissues.
Research Articles Used To Write This Article
Taunton JE, Ryan MB, Clement DB, et al. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36(2):95–101.
Bramble DM, Lieberman DE. Endurance running and the evolution of Homo. Nature. 2004 Nov;432(7015):345–52. PubMed #15549097
Lauersen JB, Bertelsen DM, Andersen LB. The effectiveness of exercise interventions to prevent sports injuries: a systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. 2014 Jun;48(11):871–7. PubMed #24100287
Bolgla LA, Malone TR, Uhl TL, Umberger BR. Hip and knee strength, EMG activity, and kinematics in subjects with patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2006 Jan;36(1):A67. PubMed #18349475
Ioannidis J. Why Most Published Research Findings Are False. PLoS Medicine. 2005 08;2(8):e124.
Noehren B, Schmitz A, Hempel R, Westlake C, Black W. Assessment of strength, flexibility, and running mechanics in men with iliotibial band syndrome. J Orthop Sports Phys Ther. 2014 Mar;44(3):217–22. PubMed #24450366
Brushøj C, Larsen K, Albrecht-Beste E, et al. Prevention of overuse injuries by a concurrent exercise program in subjects exposed to an increase in training load: a randomized controlled trial of 1020 army recruits. Am J Sports Med. 2008 Apr;36(4):663–670. PubMed #18337359
https://www.usarcent.army.mil/News/Article/1846180/us-army-physical-therapist-teaches-running-technique-to-kuwait-national-guard/#:~:text=In%20order%20to%20reduce%20risk,our%20joints%2C%E2%80%9D%20Williams%20explained.